Treating Flat Feet in Children: A Safe, Non-Surgical Roadmap
Flat feet can make children tire quickly, move less smoothly, and over time may affect their walking pattern and the way their bones and joints develop. The good news is that, in most children, flat feet can be improved without surgery if the condition is detected early and managed properly.
At Maple Healthcare in Ho Chi Minh City, clinicians assess your child’s feet using specialized arch-measuring equipment to evaluate arch height, leg alignment, and how body weight is distributed. Based on these findings, the team typically combines physiotherapy and personalized orthotics (custom foot insoles) to help support the arch, improve alignment, and optimize your child’s walking pattern.
In this article, you’ll find a step-by-step explanation of the causes, warning signs, and non-surgical treatment roadmap for flat feet in children.

Parents can perform a few simple checks at home to screen for possible flat feet in their child:

Children are reviewed regularly, and their home exercises or orthotics may be adjusted to match each stage of growth and development.


What Are Flat Feet in Children and When Is Treatment Needed?
Flat feet occur when the arch on the inside of the foot does not form properly or collapses, so the entire sole of the foot touches the floor when the child is standing. In newborns and very young children, this is usually a normal physiological stage. Many babies appear to have flat feet because of a layer of fat under the sole and because their ligaments are not fully developed yet. Parents can use the stages below as a reference:- Birth to 2 years
- Ages 2–4 years
- Ages 4–6 years
- After age 6
- The child often complains of pain or fatigue in the feet, ankles, or knees after walking or running.
- The child’s shoes wear down unevenly, especially on the inside edge of the heel.
- The child’s gait rolls inward, they trip easily, or have difficulty maintaining balance. Parents should pay attention to the alignment of the knees.
- The child avoids physical activity or is reluctant to play sports like their peers.
Table: Common Grades of Flat Feet in Children
| Grade | Key Characteristics | Typical Symptoms | Impact & Suggested Approach |
| Grade 1 | Arch only slightly lowered; arch still visible, especially when standing on tiptoes. | Little or no pain; mild fatigue after long periods of standing or walking. | Mild impact. Often improves with foot-strengthening exercises, walking barefoot on sand/grass, and light arch-support insoles. |
| Grade 2 | Arch clearly lowered; heel tilts inward (heel valgus). | Frequent pain or fatigue in the feet, ankles, knees, or hips. Gait begins to change. | Moderate impact. Usually needs personalized orthotics plus regular physiotherapy and rehabilitation exercises. |
| Grade 3 | Arch almost completely lost; foot very flat; heel tilts inward significantly (>15°). | Persistent pain, even at rest; visible foot/knee deformity; risk of “knock-knees” and possible impact on the spine. | Significant impact. Requires more intensive treatment. In some cases, surgical correction may need to be considered. |
 Signs Parents Can Check at Home
Signs Parents Can Check at Home
Parents can perform a few simple checks at home to screen for possible flat feet in their child:
- Wet footprint test Let your child wet the soles of their feet and stand on a flat surface or a piece of paper. → If the footprint shows the entire sole without an inward curve on the inner side, your child may be at risk of flat feet.
- Observe the heel (heel valgus) Look from behind: the heel tilts inward, the toes may point in a “V” shape, and the knees may angle towards each other (suggesting knock-knees).
- Watch how your child moves Your child may tire quickly when walking, walk with a limp, or avoid running and jumping activities.
Common Causes of Flat Feet in Children
Several factors can contribute to flat feet in children:- Genetics and ligament laxity Children may inherit their anatomical features from parents, including looser ligaments, making it harder for the arch to form.
- Underdevelopment or imbalance of arch-supporting muscles For example, issues involving muscles such as the tibialis posterior or peroneus longus can affect the arch.
- Mechanical factors
- Wearing very flat shoes without arch support
- Spending long periods walking or standing on hard, flat surfaces
- Being overweight or obese, which increases pressure on the feet
- Post-injury or leg length discrepancy Previous injuries or differences in leg length can change the way forces are distributed through the feet.
Types of Flat Feet
- Flexible flatfoot The arch appears when the child stands on tiptoes, but flattens when standing normally. This type often responds well to non-surgical, conservative treatment.
- Rigid flatfoot The arch is absent in all positions. In severe cases, surgical intervention may need to be considered.
Optimal Non-Surgical Treatment Approaches
The main goals of treating flat feet in children are to:- Support and encourage a more natural arch,
- Correct alignment of the ankle, knee, and hip,
- Help the child achieve a stable, balanced gait.
Chiropractic Care for the Foot, Ankle, Knee, and Hip
Chiropractic care (chiropractic adjustments) focuses on small joints in the ankle, subtalar region, knee, and pelvis—key areas that influence how forces are transmitted through the foot. Through gentle, targeted adjustments, clinicians aim to:- Restore mobility in ankle and related joints.
- Reduce inward collapse of the knees (knee valgus).
- Improve overall balance and reduce muscle tension in the legs.
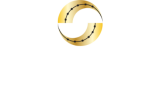
Physiotherapy and Rehabilitation
After joint mechanics are addressed, children are guided through specific exercises to:- Activate the muscles that support the arch, improving load-bearing capacity.
- Stretch the Achilles tendon and plantar fascia to improve flexibility in the heel and ankle.
- Retrain standing and walking posture to limit misalignment at the knees and hips.
- Combine modalities such as short-wave therapy, therapeutic ultrasound, or laser when there is inflammation or muscle tightness.
Personalized Orthotic Insoles
Orthotic insoles are custom-made inserts designed to fit the unique shape of each child’s feet, based on a 3D scan performed at the clinic. They can help to:- Support the arch in a more physiological position.
- Distribute pressure more evenly during standing, walking, and running.
- Reduce inward heel collapse and support joints higher up, including the knees and hips.
Follow-Up Roadmap and Progress Criteria
At Maple Healthcare, progress is monitored over time:| Stage | Expected Goals |
| 4–6 weeks | Reduced pain and fatigue; child walks and stands more comfortably. |
| 2–3 months | Improved gait; more even weight distribution; shoes show less or no uneven wear. |
| 6 months and beyond | More stable arch formation; child moves more confidently and participates in activities more easily. |
When Should Parents Consider Surgery?
Surgery is only considered in the following situations:- The child has rigid flatfoot with significant deformity.
- Pain is persistent and limits activity despite more than 6 months of appropriate conservative treatment.
Home Exercises to Support Your Child’s Recovery
Ball rolling (tennis or golf ball) Have your child sit on a chair, place the ball under the sole, and roll it back and forth along the arch for 2–3 minutes on each foot. This helps activate the plantar muscles and ease tightness in the fascia and tendons. Towel curls Place a towel on the floor and ask your child to use their toes to scrunch or pull the towel towards themselves. This exercise strengthens the muscles that help lift the arch. Short foot (arch lift) Have your child stand upright, keep the toes touching the floor, and gently lift the inner arch of the foot while holding for 5–10 seconds. This helps train the natural reflex of forming an arch. Calf stretch (Achilles stretch) Let your child stand facing a wall, step one leg back with the heel on the floor, and hold the stretch for about 30 seconds on each side. This stretch improves ankle flexibility and may help reduce heel collapse. Toe yoga Ask your child to lift the big toe while keeping the other four toes on the floor, then switch (lift the four toes while keeping the big toe down). This helps improve control of the small foot muscles and supports better neuromuscular coordination. Parents should supervise these exercises and stop if the child experiences significant pain or excessive fatigue.
Flat Feet Treatment for Children at Maple Healthcare
Maple Healthcare is a specialized musculoskeletal clinic in Ho Chi Minh City with more than 12 years of experience managing orthopedic, rehabilitation, and chiropractic conditions. Clinicians at Maple Healthcare receive advanced training (including in the United States) and use modern techniques to help children improve foot alignment and move more naturally.Five Treatment Steps at Maple Healthcare
- Comprehensive screening 3D foot scanning and in-depth assessment of leg, knee, and spine alignment to identify key contributing factors.
- Clear explanation of findings The clinician explains your child’s condition in detail and proposes an individualized care plan so parents understand each step.
- Safe, gentle manual care Chiropractic techniques and rehabilitation exercises are applied to rebalance the musculoskeletal system and gradually improve alignment.
- Personalized orthotic design Orthotics are measured, cut, and adjusted specifically for each child, supporting the arch and helping maintain straighter leg alignment during daily activities.
- Regular follow-up and close monitoring Progress is reviewed at follow-up visits, and the care plan is adjusted as needed to support more stable, long-term results.
Tips to Help Prevent or Limit Flat Feet in Children
- Choose appropriate footwear Look for shoes with some arch support and a firm heel counter to support the rearfoot.
- Maintain a healthy body weight Avoid excessive weight gain that can increase pressure on the feet.
- Encourage outdoor activity Let your child play barefoot on safe surfaces such as sand or soft grass to stimulate the foot muscles and reflexes.
- Avoid overloading at the start of treatment When treatment begins, avoid excessive running or jumping until your child’s feet and legs adapt.
- Schedule regular check-ups Follow up every 3–6 months so that treatment plans or orthotics can be adjusted as your child grows
Conclusion
Flat feet in children are not just a cosmetic issue. Over time, they can affect posture, walking pattern, and the development of bones and joints. Early detection and appropriate, evidence-informed treatment can help reduce complications and improve your child’s quality of life. At Maple Healthcare in Ho Chi Minh City, international clinicians combine chiropractic care, physiotherapy, rehabilitation exercises, and personalized orthotics to provide a gentle, non-surgical approach for many children. These methods are designed to be low-pain and very safe when used correctly. If you have questions or would like more guidance, you can leave your information in the contact form below or message the Maple Healthcare Fanpage for faster support.FAQ – Frequently Asked Questions
At what age is flat feet treatment most effective for children?
Answer: An assessment for flat feet can be appropriate at any age if you notice abnormal gait, excessive pronation, or pain. Many children respond especially well when treatment starts while the arches and alignment are still developing in the early childhood and early school years. Your clinician will look at your child’s specific stage of growth and recommend a timing and plan that fit their individual needsHow long does it take for orthotics to show results?
Answer: Many children notice reduced foot fatigue after about 6–12 weeks of regular use. More noticeable changes in arch shape and gait often appear over 3–6 months, as the arch gradually develops.Can home exercises replace orthotics?
Answer: Not completely. Exercises are important for strengthening the foot muscles, while orthotics help guide and support the arch structure. The two approaches usually work best together as part of a comprehensive care plan.When is surgery necessary?
Answer: Surgery should only be considered if the child has rigid flatfoot, persistent pain, significant deformity, and has not responded to well-conducted conservative treatment over several months. Decisions are made on a case-by-case basis.Can flat feet cause knee or back pain in children?
Answer: Yes. When the arch collapses, force transmission through the knees, hips, and spine can become unbalanced. Over time, this may contribute to knee pain, low back discomfort, or muscle fatigue around the spine if not addressed.Does walking barefoot help improve the arch?
Answer: Walking barefoot in a safe, clean environment can support overall foot health and may help arch development, especially in young children. Parents should always supervise and ensure surfaces are clean and free of sharp objects. Answer: When going outdoors, children should still wear appropriate footwear. If your child has rigid flat feet or other foot problems, it is important to seek advice from a healthcare professional before making major changes to footwear or activity.Related articles:
The Risks of Flat Feet: Signs, Identification, and Effective TreatmentMAPLE INTERNATIONAL CO., LTD
Phone: 0705 100 100
Tax code: 0311948301
Date Range: 21 - 08 - 2012
Issued: Department of Planning and Investment of Ho Chi Minh City